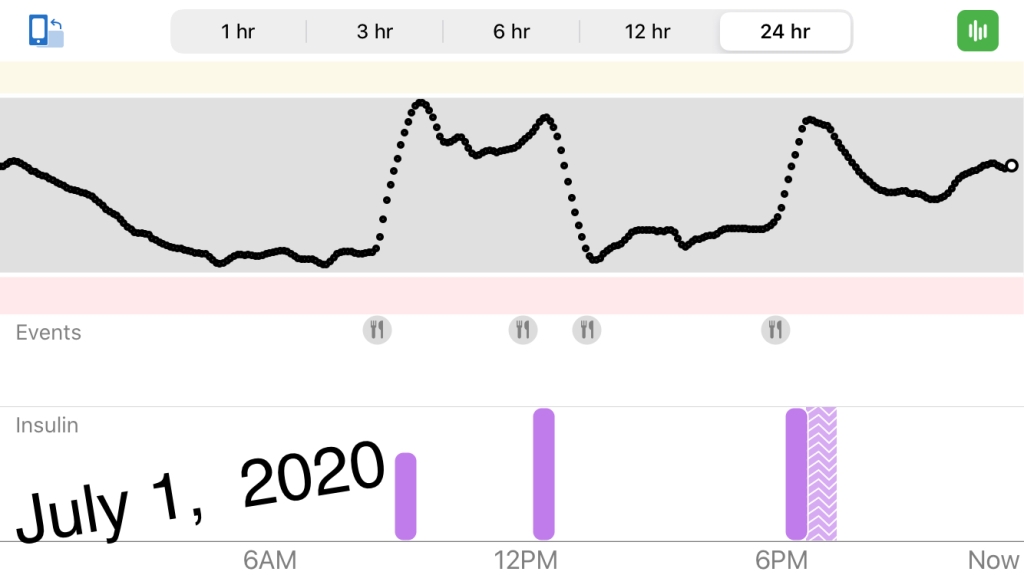
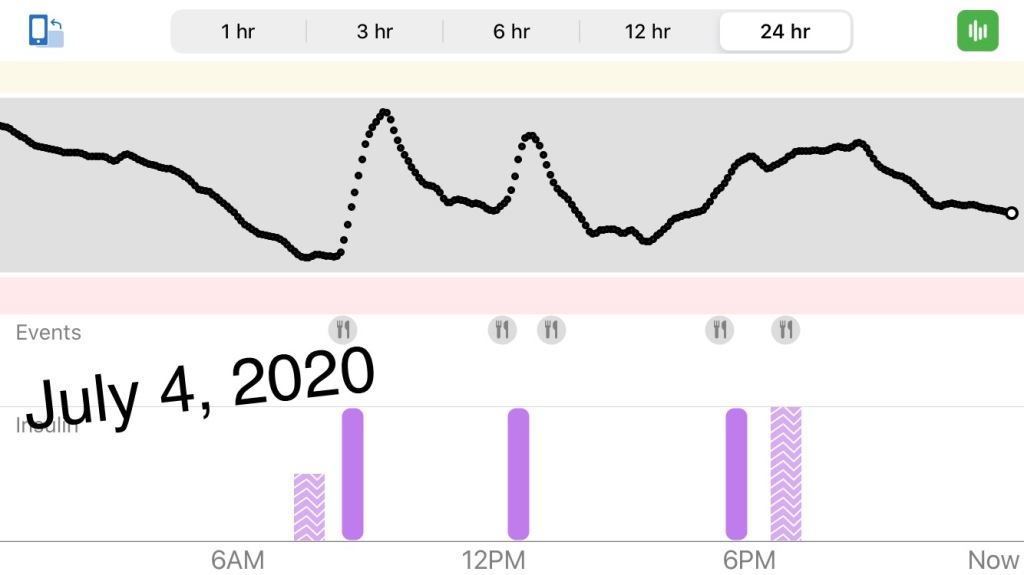
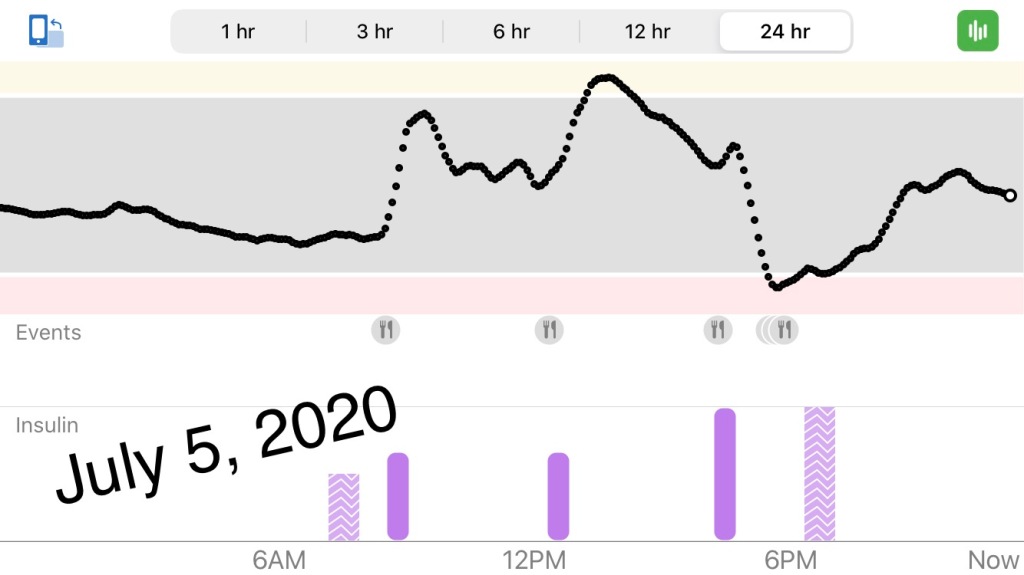
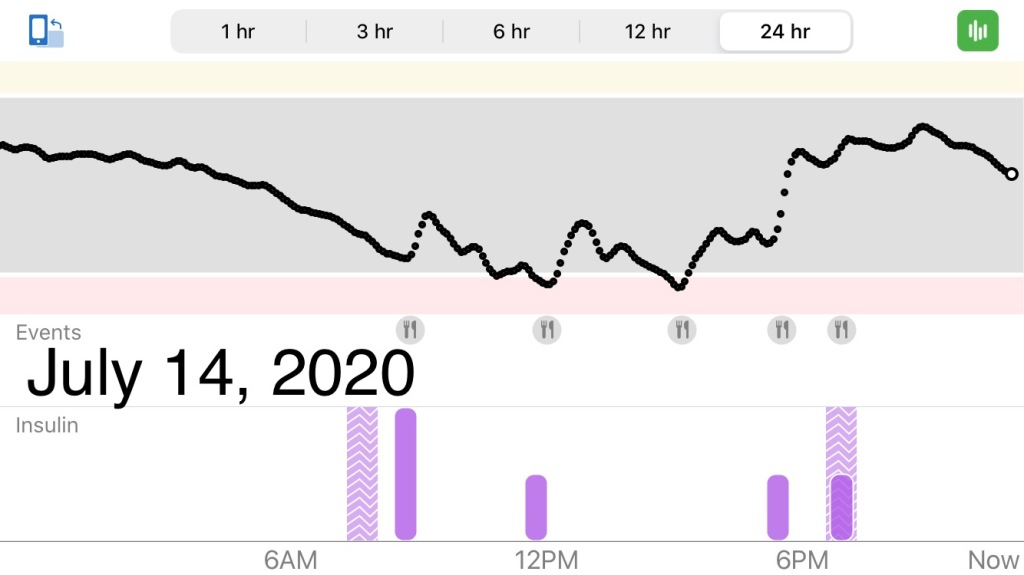
We were nearing the 4 week mark since Hannah was hospitalized and diagnosed with type 1 diabetes. We noticed the first 2 weeks, Hannah’s numbers mostly ran high. By the third week, we were settling in with the Dexcom continuous glucose monitor, and we were starting to notice some trends. Hannah would spike in the morning after breakfast and stay in the upper 200s/300s or even 400s for a while. She would just be starting to come down when we would feed her for lunch. She would climb a little, then an hour or two later she would crash into the double digits. We would watch her fall, and when she got into the 100s, 90s, 80s, we learned to give her a 10g chocolate milk which would right her ship in about 10-15 minutes. She might stay “in the grey” until dinner, when she would spike again. We would give her fast-acting insulin like we would after each meal, and we would give her the long acting insulin as we were getting ready for bed, usually between 6:30 and 6:45 at night. It was difficult to get her down from her dinner high, and she would either spend the night high or sometimes in the middle of the night we would watch her come down and wait an hour or so with a bottle in hand listening to an alarm sound every 5 minutes to see if we needed to wake a sleeping baby (really who wants to do that?) to give her a bottle she didn’t ask for to get her sugars back up. Sometimes she’d go into the morning with a decent blood sugar; sometimes she’d start the day high.
I really love how accessible our endocrinologist office is. I messaged them on Monday that I was concerned with her trends. They adjusted her insulin to carb ratio from 1:28 to 1:30.
They do weekly GoToMeeting check-ins every Wednesday night for anyone who wants to log in to ask a question; we’re never more than a week away from a live chat with someone in the office. I again expressed concern about her trends and the report they send out every Tuesday. Her estimated A1c was 10.8 😨 Like, how embarrassing to not be taking better care of her. And how scary to think about her future with an A1c so high 😥 Our doctor had mentioned at our in office appointment the week before that we might have to give her an extra Lantus dose in the morning, since the dose she was getting before bed was so low (because she’s so little) that it is likely only lasting 6-10 hours instead of 24. That made sense to me especially juxtaposed with people’s anecdotal first hand accounts I had been listening to on the Juicebox podcast, but at the time, the doctor wanted to see more days worth of Dexcom data. Since we weren’t even a week in, he wanted to wait on that. So I asked about it at this Wednesday night’s GoToMeeting check in. The nurses/educators said that we should focus on one thing at a time, so we could keep track of what’s going on. They wanted to focus on her crashes first, so stick with the new insulin to carb ratio that we altered a few days before (the aforementioned Monday message) and see how it goes.
The next day was Thursday, and I had my third diabetes education class on GoToMeeting. I again expressed my concern about her trends that seemed to not be changing despite the change in insulin to carb ratio. She still would crash everyday after lunch. They said to change her insulin to carb ratio to 1:32 or 1:34 just for lunch. But you know, sometimes when you calculate 1:28 vs 1:30 vs 1:32 or 1:34 you still end up with the same amount of insulin once everything is rounded out to the nearest half unit. And yes, I suppose we could keep giving her a 10oz chocolate milk to catch her fall everyday, but that’s no way to live – with the fear of seizure and coma everyday unless we catch her fall with a chocolate milk. Something was wrong.
After the Thursday GoToMeeting education class, she crashed again. That night after dinner she climbed up into the 400s and stayed there for HOURS. We were so frustrated. We were following their recommendations, their rules, but I couldn’t help but think there was something being withheld. Something was obviously not right. How could we live like this? Like this is her number roller coaster just because she’s little?
The parents and type 1 diabetics that were on the juicebox podcast seemed to know something, but I couldn’t quite put my finger on what it was. Something about pre-bolusing insulin before meals, which is not how we are instructed to do it with Hannah. We’re supposed to count her carbs when she’s done eating and calculate the appropriate amount of insulin and give it to her. There was something about bumping and nudging, but Hannah isn’t on a pump, so we can’t quite micromanage like the pump allows you to.
At 11:00PM on Thursday night, I was still staring at a number close to 400 which hadn’t moved in a few hours. I was supposed to get up early for a first Friday of the month at work. Desperate, frustrated, curious and defiant, I messaged Scott, the Juicebox podcast guy:
“Hello there! I’m sure you get so many messages, so I’m just throwing this out there, but my daughter was in DKA at 11 months old almost 4 weeks ago. She’s since turned 1. We have a Dexcom, but not a pump. A dental school classmate of mine recommended your podcast while we were in the hospital, so I started listening right away. I feel so guilty I pestered the pediatrician about diabetes with my older daughter but dismissed it with my second since nothing panned out with the first. We currently struggle with really high numbers and a once a day crash usually after lunch. I really do like our endo as they’re very accessible 24 hours a day by phone, messaging, weekly GoToMeeting calls, analyzing her tidepool… They say that it’s so hard because she’s so little. But like a nice line chill’n in the grey bar of the dexcom chart is like absurd to think of right now. Is this just how it is for tiny humans? Like any parent, I just want the best for her, and I’m not sure I’m ok with 400s and 50 in the same day because she’s “little.” Are we just surviving now this soon after diagnosis? Just figuring her out? Is this how all tiny humans are? Or could we be better? Happy 4th  Stay safe and well! Thanks
Stay safe and well! Thanks  “
“
He answered back! At like 12:36AM his time. “Cathy I have to get to sleep, but send me her dexcom graphs, and I’ll get back to you in the morning.”
Hopeful “to be continued…”